Direct healthcare costs are 149% higher for people with unrecognized depression compared to people without depression symptoms. The prevalence of mild to severe depression symptoms in the general population increases from 23% to 40% when accounting for people whose clinical assessments show signs of depression, but report “not experiencing depression” and “never being diagnosed with depression.” This results in a $6,269 increase in incremental healthcare costs when compared to people with minimal to no depression, according to an analysis of data from the National Health and Wellness Survey (NHWS) that was published today by Happify Health, the Intelligent Healing Company™.
This press release features multimedia. View the full release here: https://www.businesswire.com/news/home/20220207005186/en/
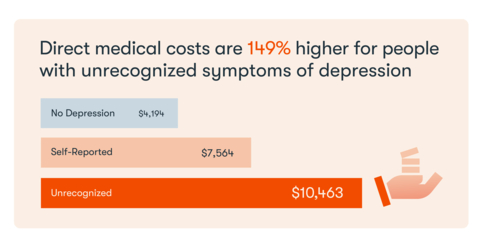
The Happify Health analysis found that the average weighted direct healthcare costs for an individual with no depression was $4,194 per year. Those costs increase to $7,564 (+80%) for people with self-reported depression and to $10,463 (+149%) for people with unrecognized symptoms of depression. (Graphic: Business Wire)
“Roughly 45% of Americans reported having a chronic health problem, which costs the United States over $3.7 trillion in direct and indirect healthcare spending each year,” according to Murray Zucker, M.D., Chief Medical Officer, Happify Health. “Our analysis demonstrates the potential to lower healthcare costs through early detection and treatment of depression—especially among people with comorbid chronic illnesses.”
The study, authored by Happify Health’s Director of Health Economics and Outcomes Research (HEOR), Anita Mohandas, MSc, MHP, was presented at ISPOR Europe 2021 in November 2021 and by Dr. Zucker at the Future of Mental Healthcare Conference in December of 2021. See the full report here.
Happify Health’s HEOR team used the NHWS data to model the incremental burden of depression symptoms at the individual and population level. The average cost per individual was weighted by the severity of depression symptoms, and across groups who self-reported having depression, and who had unrecognized depression.
Direct Healthcare Costs Impacted by Depression Symptoms
The Happify Health study found that the average weighted direct healthcare costs for an individual with no depression was $4,194 per year. Those costs increase to $7,564 (+80%) for people with self-reported depression and to $10,463 (+149%) for people with unrecognized depression.
On average, the length of time between the onset of depression and when a person receives treatment is eight years, according to a 2012 Milliman study.* Eight years of unrecognized depression would add more than $6,000 per year to an individual’s healthcare costs, resulting in an additional $50,000 in direct healthcare costs, per person.
A 2019 Government report** on untreated depression and the National Survey on Drug Use and Health*** found that people who fail to recognize their depression symptoms typically do so as a result of four key factors:
1. Lack of mental health literacy, which limits one’s ability to recognize symptoms
2. The stigma attached to seeking help for mental illness
3. An inability to perceive the illness
4. Skepticism of treatment options and preference for self-treatment
Summary of Findings from the National Health and Wellness Survey
- The prevalence of depression symptoms increases from 23% to 40% when accounting for individuals with unrecognized depression symptoms.
- The average incremental adjusted costs for someone with unrecognized depression symptoms are $6,269 higher per year compared to costs associated with individuals with minimal to no depression symptoms.
- Direct healthcare costs increase with the severity of unrecognized depression; those with mild to moderate depression symptoms had an average of $3,918 in incremental costs, compared to those with severe depression symptoms who had an average of $12,453 in incremental costs.
-
People with unrecognized depression symptoms also had a lower quality of life based on their responses to an SF6D assessment, which is a health-related quality of life metric.
- Those with mild to moderate unrecognized depression symptoms scored 13% lower on the SF6D assessment.
- Those with severe unrecognized depression symptoms scored 19% lower on the SF6D assessment.
-
The prevalence of depression among individuals with chronic conditions often exceeds 50% when unrecognized depression symptoms are factored in:
- Prevalence of depressive symptoms is 41% among people with hypertension (12% have unrecognized depression symptoms).
- Prevalence of depressive symptoms is 47% among people with Type 2 Diabetes (13% have unrecognized depression symptoms).
- Prevalence of depressive symptoms is 58% among people with heart failure (18% have unrecognized depression symptoms).
- Prevalence of depressive symptoms is 69% among people with migraines (18% have unrecognized depression symptoms).
- Prevalence of depressive symptoms is 53% among people with arthritis (15% have unrecognized depression symptoms).
- Prevalence of depressive symptoms is 42% among people with cancer (16% have unrecognized depression symptoms).
- Prevalence of depressive symptoms is 71% among people with Multiple Sclerosis (20% have unrecognized depression symptoms).
Methodology
Happify Health’s findings are based on analysis of the NHWS, which includes responses to the Patient Health Questionnaire-9 (PHQ-9) survey. PHQ-9 is a clinically validated survey that is used to measure the severity of depression symptoms in general medical settings. At a population level, scores can be used to estimate the prevalence of major depressive disorder (MDD) where scores of 10 or higher indicate a high likelihood of MDD.
- To analyze healthcare costs for people with minimal depression symptoms, Happify Health researchers looked at healthcare utilization among people who scored 4 or lower on the PHQ-9 survey and responded “no” when asked if they had experienced depression symptoms in the past 12 months.
- To identify healthcare costs for people with self-reported depression, Happify Health researchers looked at responses from people who took the PHQ-9 survey and responded “yes” when asked if they had experienced depression symptoms in the past 12 months.
- To identify healthcare costs for mild to severe depression symptoms for people who reported not having a depression diagnosis and self-reported depression status, Happify Health looked at responses from people who scored 5 or higher on the PHQ-9 survey, but responded “no” when asked if they had experienced depression symptoms in the past 12 months, and “no” to a depression diagnosis.
Direct costs were based on average healthcare utilization (all-cause utilization (inpatient, outpatient and ER visits) and mental health Rx), and indirect costs were based on presenteeism and absenteeism related losses for employed participants with depression
Note:In this study, the population with “unrecognized” and “undiagnosed depression” included individuals who responded to a survey that they had not “experienced depression symptoms in the past 12 months” and had never “received a diagnosis of depression,” but who scored greater than 4 on the PHQ-9 assessment. “Unrecognized depression” and “Undiagnosed depression” are not clinical terms, and these individuals do not necessarily meet the diagnostic criteria for major depressive disorder. The PHQ-9 is not a diagnostic tool, but is used to screen for–and assess—the severity of depression symptoms.
About Happify Health
Happify Health is The Intelligent Healing Company™. We shorten the distance between need and care by configuring personalized digital therapeutics and care solutions at scale for the modern healthcare cloud. Our platform integrates AI with empathy, making healing more personal, precise, and connected for the entire care journey. We deploy a full spectrum of clinical-grade care solutions—including Digital Therapeutics, Coaching, Community, and Well-being products—for pharma, health plans, enterprises, and individuals everywhere. For more information, visit HappifyHealth.com.
Our global platform is available in 10 languages, supports chronic conditions, and covers more than 20 million lives.
*Melek, S., & Halford, M. (2012). Measuring the cost of undiagnosed depression. Contingencies. https://www.milliman.com/-/media/milliman/importedfiles/uploadedfiles/insight/research/health-rr/pdfs/cost-of-undiagnosed-depression.ashx.
**Report to Congressional Requesters. Research on Health Care Costs of Untreated Conditions is Limited. February 2019. GAO-19-274U. https://www.gao.gov/assets/gao-19-274.pdf.
***SAHMSA. The National Survey on Drug Use and Health : 2019 National Survey on Drug Use and Health ( NSDUH ). SAMHSA – Substance Abuse and Mental Health Services Administration (2019).
View source version on businesswire.com: https://www.businesswire.com/news/home/20220207005186/en/
